4
WORLD GASTROENTEROLOGY NEWS OCTOBER 2018
Editorial | Expert Point of View | Gastro 2018 | WDHD News | WGO & WGOF News | WGO Global Guidelines | Calendar of Events
Which foods are incriminated by
IBS patients? Effect of FODMAPs
Presently the most incriminated foods
in IBS are the so-called FODMAPs.
This is a quite recent acronym for
fermentable sugars and alcohols.
FODMAP stands for Fermentable
Oligosaccharides, Disaccharides,
Monosaccharides and Polyols.3 Indeed,
there are many empirical reports
of worsening IBS symptoms related
to fermentable food. Fermentable
oligosaccharides include very poorly
absorbed carbohydrates like short
chain fructooligosaccharides or fructans;
galacto-oligosaccharides; lactose;
fructose; polyols include sorbitol,
xylitol, maltitol etc. These compounds
are found in many foods like cereals,
legumes, vegetables, fruits.
Typical vegetables and legumes
high in FODMAP are: garlic, onions,
artichoke, asparagus, beans, banana,
beetroot, cauliflower, celery,
mushrooms, peas etc. Fruits high in
FODMAPS are apples, dates, mango,
pears, pine-apples, prunes, raisins,
watermelons etc.; wheat; spices. It is
therefore advisable to recommend to
patients susceptible to be intolerant
to high FODMAPs content food to
avoid these.4
The foods poor in FODMAPS are:
vegetables and legumes: broccoli,
carrots, cucumber, lettuce, potatoes,
pumpkins, tomatoes; fruits: green bananas,
berries, grapes, lemon, papaya;
cereals: corn. We should recommend
these foods to patients with IBS.
With respect to the role of FODMAPs
in the managing of IBS
symptoms, there is a growing body of
evidence supporting the efficacy of the
low FODMAP diet.5 Advising our
patients with IBS to decrease their intake
of FODMAPs has been reported
to reduce abdominal symptoms in 2
to 4 weeks.6
There are also other opinions
stating that it is not only the composition
of food, i.e. the FODMAPs
composition is important, but also the
regular healthy dietary advice7: regular
meals, low consumption of caffeine
and alcohol, fat avoidance. There are
also concerns about an excessive low
FODMAPs diet, which could lead to
hypocalcemia, low intake of fibers and
changes in gut microbiota.8 Note
that experts suggest that patients
adhere to a strict FODMAP diet for
no more than a few months.
General dietary factors
Beside the fermentable carbohydrates
and alcohols, general dietary
recommendations are important and
patients should respect them.
Regular meals
Like for healthy people or for many
other patients, having regular meals
at precise hours, in a comfortable environment,
without hassles and stress
are important for the well-being.
Coffee and tea
Both are very frequently consumed
foods; in patients with associated
gastroesophageal reflux disease, patients
should avoid coffee. Otherwise
there is no reason to forbid coffee in
IBS patients (except for the few who
claim diarrhea after coffee ingestion).
Tea has also no implication in IBS;
if digestive symptoms occur after tea
consumption, the nature of the symptoms
should be clarified. Use of coffee
and tea should be left to the options
of the patients.
Alcohol
In alcohol-consuming IBS patients,
the use should not be forbidden if it is
not linked to symptoms (empirically
more frequently observed diarrhea).
Of course the use of alcohol should be
in generally accepted amount and not
in excess.
Gluten
With the actual interest on gluten
sensitivity induced by mass-media,
many IBS patients give up from own
initiative the consumption of gluten.
However, there is no argument to
forbid gluten unless there is associated
sensitivity, because the role of
gluten in IBS is not at all proven.9
Even if patients affirm they feel better
with a gluten-free diet, the role of the
placebo effect has to be considered.
It is recognized now, however, that
there is an entity of non-celiac gluten
hypersensitivity.
The alimentary pyramid of IBS
patients
Given the importance to advise the
patients what to eat, and not only
what to avoid, we created a pyramid
of food to be recommended to
IBS patients, according to available
evidence.5
According to this pyramid, the food
that IBS sufferers should consume are
presented in table 2.
General recommendations instead
of conclusions:
Diet represents a major point of
attack in the management of IBS.
Dietary recommendations should
be individualized, based on evidence
Continued from first page.
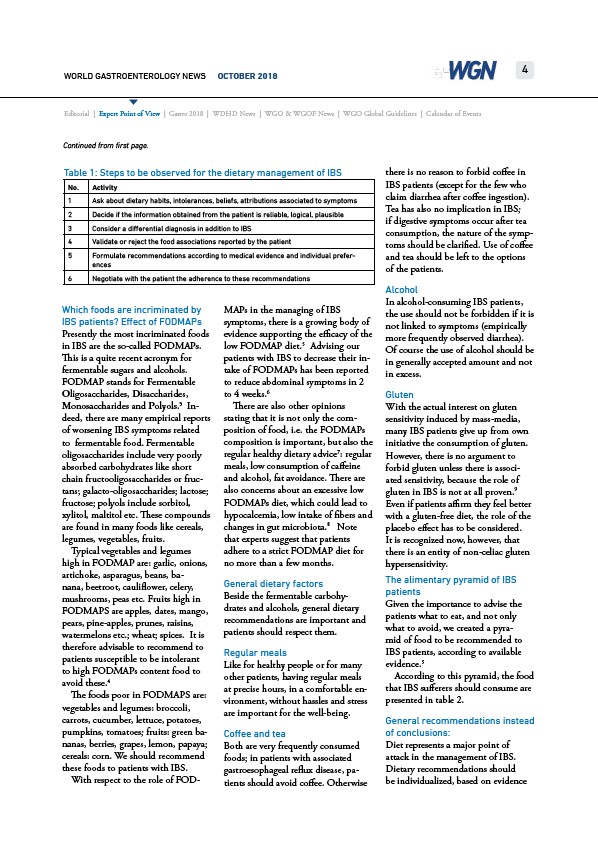
Table 1: Steps to be observed for the dietary management of IBS
No. Activity
1 Ask about dietary habits, intolerances, beliefs, attributions associated to symptoms
2 Decide if the information obtained from the patient is reliable, logical, plausible
3 Consider a differential diagnosis in addition to IBS
4 Validate or reject the food associations reported by the patient
5 Formulate recommendations according to medical evidence and individual preferences
6 Negotiate with the patient the adherence to these recommendations